Release date: 2017-04-27
Cell therapy has not been very successful in combating solid tumors, in part because it is difficult to deliver anti-cancer T cells to tumors.
A strategy developed by Fred Hutchinson Cancer Research Center researchers can help you. The team is equipped with a synthetic scaffold loaded with anti-cancer T cells and a mixture of nutrients that keep the cells healthy and cause cancer.
The study, which will be published in the Journal of Clinical Investigations on April 24, shows that stents containing T cells are more effective in reducing tumors in pancreatic cancer and melanoma mouse models than T cells delivered by injection.
Dr. Matthias Stephan, senior author of Fred Hutch and a biomaterials expert, said: "The key to our stent is that it is more than just a structure. The components we design for these stents include the best combination of stimulating factors and other ingredients. T cells survive and proliferate and maintain sustained combat against cancer cells."
In the study, the researchers loaded the scaffold into chimeric antigen receptors or CART cells, which were engineered in the laboratory to look for proteins specific for cancer cells and then destroy the cells.
T cells are very picky, you can't inject them into the tumor and let them work. If they are not in an environment with sufficient nutrients and a proper elimination of pollution, they will die within a few days. In addition, tumors release their own defense chemicals to prevent T cells from working.
Stephen and his team designed a comfortable environment to overcome these obstacles.
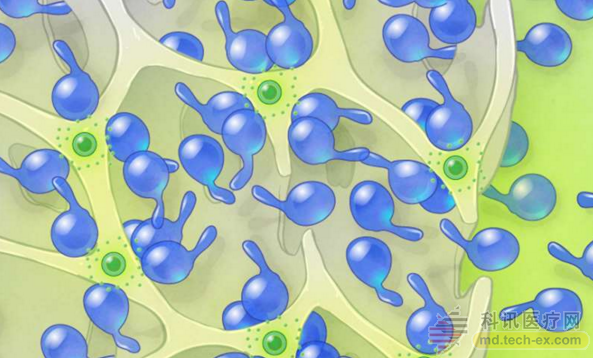
This viscous, spongy, soluble biopolymer scaffold consists of tiny pores that can be made in any size or shape. Stephan and his team at MIT and the University of Washington used scaffolding to load CAR-T cells and proteins to keep T cells healthy, allowing them to grow quickly and attack tumors quickly. The mixture also includes a substance called a STING agonist that increases the immune response to eliminate adjacent cancer cells that are not recognized by CAR-T cells.
Stephan said that when placed on a tumor in a mouse, the scaffold shifts the tumor environment from inhibition to a state that allows and effectively controls disease progression.
There is still a long way to go before this technology can be applied to patients. The next step is through clinical trials, and Stephen is looking for an industry collaborator to develop and commercialize the technology. It requires FDA approval.
However, if these steps are successful, Stephan believes that genetic analysis of the patient's tumor tissue will reveal the protein composition of the tumor. The scaffold can then be fabricated from a mixture of T cells and other components designed to target a variety of tumor proteins in a particular tumor of a patient. After about a week, the scaffold will dissolve, so no additional surgery is needed.
Because CAR-T cells are designed to continue to divide and grow to maintain long-lasting anti-cancer combat, patients may not need more treatment after stent implantation.
“It's like igniting a spark on a tumor,†Stephan said. By placing CAR-T cells on the tumor, they produce initial scintillation, grow immediately and attack the tumor. The immunopotentiator provided by other substances in the scaffold then adds fuel to the growing flame. The second wave of anti-tumor flame develops at a slower rate than the initial spark, but it keeps the flame.
Similar scaffolds made of biomaterials are used to deliver regenerative drugs to repair body tissues such as bones and cartilage. The surgeon places the stent on the injury site and the drug spreads out for repair.
Researchers have attempted to design stents that contain topical anti-tumor immunotherapeutics to protect patients from the broad and toxic effects of chemotherapy.
“This is a surgeon's tool,†Stephen said. He saw that bracket technology has additional uses:
1. Palliative care for patients who do not or do not want surgery, but can benefit from tumor shrinkage;
2. Reduce large tumors so that the surgeon can remove them;
3. After surgical removal of the tumor, insert the stent to dry any remaining cancer cells, reducing the chance of cancer recurrence.
Source: Noble
China leading manufacturers and suppliers of Medical Adhesive Tape,Medical Hypoallergenic Tape, and we are specialize in Medical Breathable Tape ,Medical Tape, etc.
Medical Adhesive Tape,Medical Hypoallergenic Tape,Medical Breathable Tape ,Medical Tape,Sports Tape,PU/Non Woven Fixing Tape,Non-woven Tape,Transparent Pe Tape,Silk Tape,Sawteeth,Zinc Oxide Adhesive Tape,Silk / Zinc Oxide Perforated Plaster
Surgimed Medical Supplies Co.,Ltd , https://www.surgimedcn.com